Advancements in regenerative medicine have brought forth exciting breakthroughs in various fields, and dentistry is no exception. One such breakthrough revolves around Platelet-Rich Plasma (PRP), a natural elixir derived from our own blood, and its remarkable ability to induce autophagy and promote regeneration in human dental pulp cells. In this blog, we’ll delve into this cutting-edge research, shedding light on the potential of PRP to revolutionize dental treatments.
Understanding Dental Pulp Regeneration
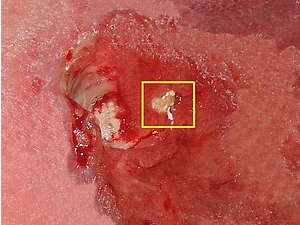
Dental pulp is the soft tissue within the tooth that contains blood vessels, nerves, and connective tissue. When dental pulp becomes damaged due to injury or infection, it can lead to discomfort and even tooth loss. The conventional treatment for such cases often involves root canal procedures. However, the concept of regenerating dental pulp offers an enticing alternative.
Autophagy: Nature’s Recycling Mechanism
Autophagy is a cellular process in which cells break down and recycle damaged or dysfunctional components, contributing to cellular health and maintenance. Recent research has revealed that autophagy also plays a vital role in tissue regeneration and repair.
The Role of PRP in Dental Pulp Regeneration
PRP, with its concentration of growth factors and bioactive molecules, has the potential to stimulate cellular processes like autophagy and regeneration. Here’s how it works:
- Induction of Autophagy: Studies have shown that PRP can trigger autophagy in dental pulp cells. This process clears out damaged components, allowing the cells to rejuvenate and become more responsive to regenerative cues.
- Stimulation of Regeneration: PRP’s growth factors, such as platelet-derived growth factor (PDGF) and transforming growth factor-beta (TGF-β), activate signaling pathways that promote cell proliferation, differentiation, and tissue regeneration. In the context of dental pulp, this could lead to the growth of new, healthy pulp tissue.
Implications for Dentistry
The potential impact of PRP-induced autophagy and regeneration in dental pulp cells is immense:
- Minimizing Invasive Procedures: If PRP can effectively stimulate dental pulp regeneration, it could offer a less invasive alternative to traditional root canal treatments, potentially preserving more of the natural tooth structure.
- Accelerated Healing: PRP’s ability to enhance autophagy and regeneration might accelerate the healing process for dental injuries, reducing the recovery time for patients.
- Personalized Dental Care: As PRP is derived from the patient’s own blood, it offers a personalized approach to treatment, minimizing the risk of adverse reactions.
- Future Innovations: The research into PRP’s effects on dental pulp cells opens doors for further innovation in dental regenerative therapies, paving the way for novel treatments that were once considered science fiction.
The synergy between Platelet-Rich Plasma, autophagy induction, and dental pulp regeneration holds tremendous promise for the future of dentistry. As science continues to unravel the intricate mechanisms at play, the potential to transform the way we approach dental treatments becomes increasingly evident. Imagine a future where damaged dental pulp can be regenerated, preserving smiles and oral health in a remarkably non-invasive and personalized manner. The journey from research to application is an exciting one, and the prospects are undoubtedly brighter than ever before.