History
Platelets were first discovered in 1842. In 1882, the Italian physician J.B. Bizzozero discovered that they played an important role in the haemostasis of blood vessels after injury and first gave the name platelets. In 1906, platelets were identified as small pieces of cytoplasm shed from megakaryocytes in the bone marrow. Platelets are smaller than red blood cells and white blood cells, measuring 1.5-4 microns long and 0.5-2 microns wide. Healthy adults have 100,000-300,000 platelets per cubic millimetre of blood, with one third of platelets normally stored in the spleen.
Platelets, or thrombocytes, have a normal value of 100,000 – 400,000/μ1. The central part of the platelet has blue-purple granules, called granulomere, and the peripheral part has a homogeneous light blue colour, called hyalomere. Under electron microscopy, platelets have a sugar-coated membrane surface and no nucleus inside the cell, but there are organelles such as tubule tracts, mitochondria, microfilaments and microtubules, as well as platelet granules and glycogen granules, etc. Platelets are only found in mammalian blood.
Structure
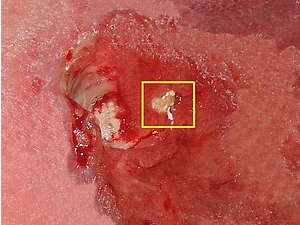
The platelet structure is complex. In brief, the platelets are structured in three layers from the outside to the inside, i.e. the outer membrane, the unit membrane and the submembrane microfilament structure, which is the first layer; the second layer is the gel layer, where microfilaments and microtubules are seen parallel to the surrounding area under electron microscopy; and the third layer is the microorganelle layer, which has mitochondria, dense vesicles and residual nuclei.
Generation
Haematopoietic stem cells undergo directed differentiation in haematopoietic tissue to form primitive megakaryocytes, which in turn become mature megakaryocytes. Mature megakaryocytes form numerous depressions on the surface of their membranes, which extend into the cytoplasm, and adjacent depressed cell membranes fuse with each other at the depth of the depressions, separating part of the megakaryocyte cytoplasm from the parent body. Eventually these components, surrounded by the cell membrane and separated from the cytoplasm of the megakaryocyte, detach from the megakaryocyte and enter the circulation as platelets via the blood sinusoids in the bone marrow haematopoietic tissue. The newly generated platelets first pass through the spleen, where about 1/3 of them are stored. The stored platelets can be freely exchanged with those entering the circulating blood to maintain a normal amount in the blood. Platelets live for about 7 to 14 days and most of the senescent platelets are removed in the spleen.
Features
The surface of platelets is rich in glycoproteins and some enzymes, which are plasma components that are specifically adsorbed on the platelet surface, and are also reactive sites for platelet adhesion and aggregation. Common surface markers for platelet flow assays are CD41 (gp IIb/IIIa), CD42a (gp Ⅸ), CD42b (gp Ⅰb) and CD61 (avb3, a bilirubin receptor). A number of new markers appear on the surface of activated platelets, the 2 main ones, PAC-1 (activated IIb/IIIa) and CD62p (p-selection), which are now widely used for clinical detection of activated platelets. There are also CD31 (PECAM) and CD63 (a lysosomal antigen), which are also useful as two markers of platelet activation.
Biological functions
The main function of platelets is to clot and stop bleeding and to repair broken blood vessels. There are various mechanisms by which the haemostatic and coagulation effects occur when blood is injured and bleeding, as follows.
- Constriction of blood vessels, which helps to stop bleeding temporarily
- Formation of haemostatic clots, blocking the rupture of blood vessels
- The coagulation effect of platelets
- Release of antifibrinolytic factors, inhibiting the activity of the fibrinolytic system
- Nourishing and supporting capillary endothelium
Without platelets, there is no immune response
When a virus attacks our body, inflammation occurs, which triggers an immune response in the body. White blood cells leave the bloodstream to migrate into the tissues surrounding the area of inflammation. The first cells to be recruited within a few hours are neutrophils, followed by inflammatory monocytes as a backup. The neutrophils emerge at the endothelium of the blood vessels at the site of inflammation. They adhere to its wall and then migrate outside the vessel to reach the damaged tissue and fight infection.
Normally, the patrolling monocytes do not come into contact with platelets. Platelets are free to swim in the blood. But once inflammation occurs, platelets interact directly with the patrolling monocytes, releasing the CCN1 protein bound to the vascular endothelium. The increased amount of CCN1 is necessary for the recruitment of resident monocytes and their patrolling activity.
In the absence of platelets in the blood during a viral attack, CCN1 levels will not rise and will not be able to recruit patrolling monocytes and will not be able to recruit neutrophils or inflammatory monocytes. Platelets are the first component of the immune defence recruitment cascade pathway. Without platelets, there is no immune response.