Knee meniscus injuries are more common in older adults, with more than 80 percent of people over the age of 75 found to have knee meniscus injuries during routine physical exams. However, according to news reports, doctors say that meniscal injuries are not just exclusive to the elderly, but young people are also a major group of people who suffer meniscal injuries, mostly caused by excessive or poor exercise.
- What is the meniscus? What does it do?
The meniscus is an important structure of the knee joint, as shown in the knee joint section below. It is located between the tibia and the femoral condyle platform, and its cross section is triangular in shape, which has the function of transmitting load and stabilizing the joint.
The meniscus is a crescent-shaped cartilage structure that is flexible, divided into two parts: the medial and lateral parts, and a triangular structure that is thick on the outside and thin on the inside when viewed from the side, fitting into the femoral condyle on top and the tibial plateau on the bottom.
The meniscus is very important to the body as it not only stabilizes the knee joint, but also has a spring-like shock absorption effect that helps reduce the vibration between the femur and tibia when we fall from a height.
In addition, the meniscus has a sliding and pressure distributing effect. It sits between the joints and secretes and distributes synovial fluid, thus spreading the pressure on the joint and making it more flexible.
- How can I determine for myself if a meniscal injury has occurred? What are the typical symptoms?
When you have the following symptoms, your meniscus may have been damaged:
Pain: pain and swelling in the knee when squatting and squatting.
Rattling: Some people feel a “tearing sound” or “popping when walking” when the joint moves.
Card: when walking or going upstairs, the knee joint is stuck, can not bend and straighten; or even “limp leg” can not stand up normally.
The most common cause of meniscus injury is trauma. The most likely cause of meniscus injury is extension and twisting activities, such as a sudden twist when falling from a height, and the meniscus may be caught in the middle of the joint and unable to move. Unlike other injuries, the meniscus is divided into medial and lateral, and it is often damaged on one side of the meniscus, manifesting as pain on one side. Another typical symptom of a meniscal injury is interlocking symptoms, where the patient has a feeling of the knee being stuck during activities such as walking and squatting, which may be relieved by activity.
- What are the treatment options for meniscus injuries?
Common meniscal injuries include longitudinal tears, oblique tears, transverse tears, basket-like tears, laminar tears, complex tears, etc.
Different meniscus injuries require different treatment methods in conjunction with clinical symptoms. Many less severe meniscus injuries may be asymptomatic. In this case, the patient usually needs to limit the amount of activity and refrain from strenuous exercise, and no other treatment is required. In addition, muscle strengthening exercises are needed to ensure joint stability, such as practicing leg lifts and weight-bearing leg hooks. If a patient with a meniscus injury has symptoms, such as pain when walking or running, that interfere with life and sports, treatment is needed. The most common treatment for meniscal injuries is minimally invasive surgery, which involves trimming, suturing, grafting, or even removal of the meniscus for different injuries. Minimally invasive knee arthroscopy is most commonly used to repair the meniscus by making a 1cm incision in the front and back of the knee, as well as inside and outside the knee, depending on the location of the injury. Lubricant (sodium vitrate) can also be injected into the joint cavity, and the latest treatment can be localized with PRP (platelet-rich plasma). Among other things, meniscal transplantation is rare and is usually only available to young people whose knee and articular cartilage are in good condition, and it is also necessary to find the right size meniscus to be donated. When the meniscus is too damaged to be repaired or sutured and continues to damage the joint, it is removed as a last resort to relieve symptoms.
- How does PRP treat meniscus injuries?
Platelet-rich plasma (PRP) is a blood product obtained by centrifugation of the patient’s own blood. Its platelet concentration is three to eight times higher than that of platelets in whole blood, and it can release a large amount of endogenous growth factors, making it an important source of growth factors and strong repair ability for bone and soft tissues, and is widely used in clinical practice. Previously, there is a large amount of literature proving that PRP can stimulate growth factors and have a regulatory effect on inflammatory factors, and that PRP can effectively maintain the metabolism of articular cartilage and protect chondrocytes in patients, achieving the effect of promoting cartilage healing.
Treatment modality
- Local treatment: PRP preparation is performed by centrifugation twice, and the prepared platelet-rich fraction of blood is selected and injected into the patient’s knee joint with a syringe.
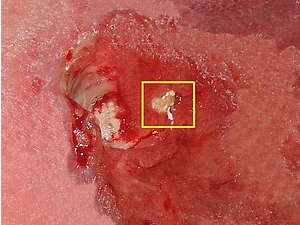
- Arthroscopy combined with PRP treatment: It has been proposed in the literature that arthroscopic treatment of patients with meniscal injury with osteoarthritis, combined with PRP treatment, can achieve better clinical results. The reason is that arthroscopic surgery is a minimally invasive surgery, which not only can correct the clinical diagnosis and reduce the chance of misdiagnosis and omission, but also can accurately determine the type, location and degree of meniscal injury, and also can discover whether there is joint attachment injury, which is conducive to the operator’s reasonable choice of surgical method and the maximum preservation of the normal tissue and morphology of the meniscus, so that the stability of the joint capsule around the meniscus can be maintained and the patient can retain The knee function is preserved. On the basis of this, PRP treatment is combined with PRP, and the growth factors in PRP have a positive effect on the injured meniscus. Numerous experiments have confirmed that PRP can maintain the balance of articular cartilage metabolism, protect chondrocytes and promote healing. In addition, PRP is injected directly into the lesion to induce chondrocyte regeneration and repair, regardless of the presence or absence of blood supply to the red and white areas of the meniscus, thus maximizing the recovery of the meniscus and further enhancing the therapeutic effect.
Related Research
Autologous PRP technology has been reported to promote tissue healing since the 1970s and has been successfully applied in maxillofacial surgery, orthopedics, orthopedics, foot and ankle surgery, etc. PRP is equivalent to concentrated platelets, and the platelet content in 5 mL of plasma is more than 106/μL. Its mechanism of action is to inject high concentrations of growth factors, cytokines and other bioactive proteins into the injured tissue to maximize tissue healing. The mechanism of action of PRP is to inject high concentrations of growth factors, cytokines and other bioactive proteins into injured tissues to maximize tissue healing and maintain internal environmental homeostasis. Numerous in vivo and in vitro experiments have confirmed that PRP has a positive effect on improving meniscus cell activity and cell regeneration, as it contains a large amount of fibrin, which provides a scaffold for meniscus repair. In a controlled study by He Hanliang et al. on 28 patients after arthroscopic meniscal repair, 14 patients were combined with PRP and the follow-up ranged from 3 to 12 months, and the Lysholm score and KOOS osteoarthritis score of patients in the PRP group were significantly higher than those in the control group. Chen Yushu et al. suggested that PRP can promote chondrocyte proliferation and extracellular matrix accumulation to repair cartilage injury, which has good efficacy in osteoarthritic knee injury. a Hamid et al. found that PRP with rehabilitation exercises significantly shortened the time required for patients to return to normal exercise and reduced the pain by an RCT that included 28 patients with acute cord muscle injury. severity.
Many studies have shown that PRP combined with arthroscopic meniscoplasty is effective in treating meniscal injuries in the elderly knee, effectively relieving postoperative pain, promoting functional recovery of the knee, reducing serum BGP, IGF-I, and MMP-1 expression levels, and reducing complications, and can be promoted for clinical use.