In the realm of regenerative medicine, Platelet-Rich Plasma (PRP) has emerged as a promising tool for promoting tissue repair and regeneration. Among its various applications, PRP’s potential to support the proliferation and redifferentiation of chondrocytes—the primary cells responsible for maintaining cartilage—has garnered significant attention. In this article, we delve into the fascinating world of PRP and its role in nurturing chondrocyte growth and redifferentiation during in vitro expansion.
Understanding Chondrocytes and Cartilage Regeneration
Chondrocytes are specialized cells found in cartilage, a connective tissue that cushions and supports joints. Cartilage has limited self-repair capabilities due to its avascular nature, making the treatment of cartilage injuries or degenerative conditions like osteoarthritis a complex challenge. This is where the potential of PRP comes into play.
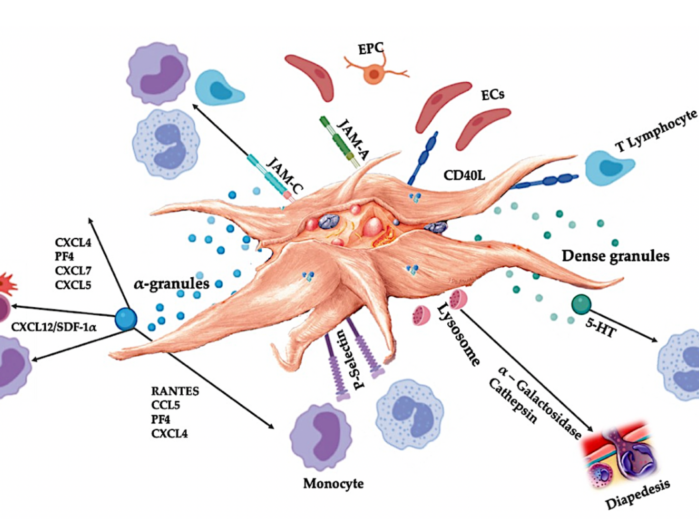
The Science Behind PRP
PRP is derived from a patient’s own blood and is rich in growth factors, cytokines, and other bioactive molecules that play a crucial role in tissue repair and healing. When PRP is applied to a damaged area, it stimulates the body’s natural regenerative processes, promoting cell proliferation and tissue remodeling.
PRP and Chondrocyte Expansion: A Synergistic Approach
Researchers have been exploring PRP’s effects on chondrocyte growth and redifferentiation, particularly in in vitro (laboratory) settings. Here’s how PRP supports these processes:
- Proliferation: PRP’s growth factors, such as platelet-derived growth factor (PDGF) and transforming growth factor-beta (TGF-β), create an environment conducive to chondrocyte proliferation. These growth factors signal chondrocytes to divide and multiply, which is crucial for generating a sufficient number of cells for tissue engineering or transplantation.
- Redifferentiation: In degenerated or injured cartilage, chondrocytes can lose their specialized properties and transition to a more fibroblastic phenotype. This transition impairs cartilage function. PRP’s bioactive components help steer chondrocytes back toward their mature, redifferentiated state. This redifferentiation is critical for regenerating healthy, functional cartilage tissue.
- Extracellular Matrix Formation: Chondrocytes are responsible for producing the extracellular matrix (ECM) that gives cartilage its structure and resilience. PRP has been shown to enhance the synthesis of ECM components, such as collagen and proteoglycans, aiding in the creation of a suitable microenvironment for chondrocyte growth and function.
Implications for Regenerative Medicine
The synergy between PRP and chondrocytes opens doors for various applications:
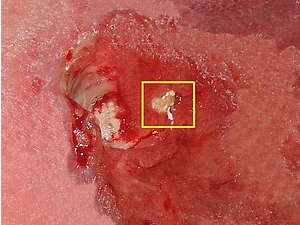
- Cartilage Tissue Engineering: PRP can be integrated into scaffolds or matrices for culturing chondrocytes, improving their proliferation and redifferentiation potential. This approach is particularly valuable for developing functional cartilage grafts for transplantation.
- Osteoarthritis Management: Osteoarthritis is characterized by cartilage degeneration. Utilizing PRP to enhance chondrocyte activity in vitro could lead to innovative treatments that help slow down or even reverse the progression of the disease.
- Enhanced Joint Repair: The combination of PRP and cultured chondrocytes holds promise for improving the outcomes of surgical procedures such as autologous chondrocyte implantation (ACI) or matrix-induced autologous chondrocyte implantation (MACI).
The convergence of platelet-rich plasma and chondrocyte biology represents a remarkable advancement in regenerative medicine. By fostering chondrocyte proliferation, redifferentiation, and extracellular matrix formation, PRP offers a pathway to address the challenges of cartilage injuries and degeneration. As research continues to uncover the intricate mechanisms at play, the potential for PRP to revolutionize the field of cartilage regeneration remains tantalizing. Through careful study and innovative application, the collaboration between PRP and chondrocytes may usher in a new era of effective treatments for joint-related ailments and beyond.