Introduction: Diabetic foot ulcers are a painful and potentially debilitating complication that arises in individuals living with diabetes. These ulcers, characterized by slow wound healing and a high risk of infection, pose a significant challenge to both patients and healthcare providers. In recent years, a novel approach using autologous Platelet-Rich Plasma (PRP) has emerged as a beacon of hope in the treatment of diabetic foot ulcers. This blog explores how PRP is revolutionizing wound care and offering a new lease on life for those affected by this condition.
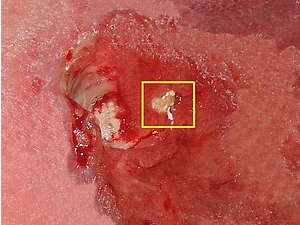
Understanding Diabetic Foot Ulcers: Diabetes, a chronic condition affecting millions worldwide, can lead to various complications, including nerve damage and poor blood circulation. These complications increase the likelihood of foot injuries going unnoticed and impair the body’s ability to heal. Diabetic foot ulcers are open sores that form due to a combination of factors, such as reduced sensation, diminished blood flow, and impaired immune response. The slow healing process puts individuals at risk of infections that could lead to serious complications, including amputation.
Enter Autologous Platelet-Rich Plasma (PRP): Platelet-Rich Plasma, a regenerative therapy derived from the patient’s own blood, has garnered attention as a potential game-changer in the treatment of diabetic foot ulcers. PRP contains a concentrated mix of growth factors, cytokines, and healing-promoting components that have the potential to expedite wound healing and improve tissue regeneration.
The PRP Healing Process: The journey of utilizing PRP for diabetic foot ulcers begins with a simple blood draw. The collected blood is then processed to extract a concentrated solution rich in platelets. These platelets are the superheroes of the healing process, releasing a cascade of growth factors that stimulate tissue repair, angiogenesis (formation of new blood vessels), and collagen production. When applied to the ulcer, PRP’s therapeutic potential comes into play.
Evidential Success: Research into the use of PRP for diabetic foot ulcers has shown promising results. Studies have reported accelerated wound closure, reduced infection rates, and improved overall healing outcomes in patients treated with PRP. The regenerative properties of PRP not only aid in wound closure but also contribute to minimizing scarring and optimizing tissue quality.
A Personalized Approach: One of the compelling aspects of PRP therapy is its personalization. Since PRP is derived from the patient’s own blood, the risk of adverse reactions or complications is minimized. This makes PRP an attractive option, especially for individuals with diabetes, who may already be dealing with a host of health challenges.
Collaborative Care: It’s important to note that PRP therapy for diabetic foot ulcers is most effective when integrated into a comprehensive care plan. Collaborative efforts between healthcare professionals, including wound care specialists, endocrinologists, and podiatrists, ensure that the treatment aligns with the patient’s overall health needs.
Autologous Platelet-Rich Plasma represents a beacon of hope for individuals living with diabetic foot ulcers. By harnessing the body’s own regenerative capabilities, PRP therapy offers a novel approach to wound healing that has the potential to transform lives. While research continues to unfold, the remarkable progress in this field hints at a brighter future for those battling the complex challenges of diabetic foot ulcers. As science and innovation march forward, PRP stands as a testament to the power of leveraging the body’s inherent ability to heal and regenerate.